Long-acting reversible contraception
We asked:
"Long-acting reversible contraception (LARC) includes the contraceptive coil and contraceptive implant. The sexual health service will work with primary care to offer provision across the city of York. The service will work with the public health team to agree a limit on the number of coils and implants fitted based on previous years data.
Do you agree with this proposal?"
In this case the majority of answers were “no” (57.89%) to agreeing a limit on the number of LARC’s offered.
| Response | % of respondents |
|---|---|
| Yes | 21% |
| No | 57.89% |
| Don't know | 21% |
Over a quarter of respondents didn’t answer the question, but 40 people commented on this question and it appeared to be the most controversial.
Comments included:
"This is preventing freedom to choose a method of contraception based on 'availability'."
"Give sexual health the full budget/contract as people can’t get appointments with a qualified person at GPs."
"This is an absolutely disgusting and sexist proposal. This should be needs led and not funding led."
"This seems like a very old fashioned solution to address this aspect of women's health. Research shows that women's health is seldom prioritised and usually poorly researched. Is this really the best you have to offer to the women of York?"
"Look elsewhere! Contraception should not be a luxury or on a first come first served basis."
"There should absolutely not be a limit on the number of LARCs. Anyone who wishes to use these should be able to. Further, the sexual health team are far more experienced at fitting these and the option to see them, rather than your primary care provider, should still exist."
"As GPs have such a long waiting list for anything to do with coils/implants, could their budget be moved across to sexual health to fit them?"
"It's not clear from this proposal whether fewer devices would be fitted in total, or whether the proposal is merely to limit the number fitted by the service, with the balance taken up by primary care."
"Primary care is already very stretched, and this should be planned very carefully to ensure that work is not merely being shifted from one under funded, stretched service to another."
"GPs although designated as contraceptive specialists are not all up to date and my experience has led to me having several coil appointments with a GP and then get sent to Monkgate. What a waste of everyone’s time. Now you’d be lucky to get a GP appointment in under 5 weeks for my group of practices."
"I can't come up with an alternative, but the idea of capping the amount of care provided is concerning."
"This disadvantages women. There needs to be collaboration with local GPs to head the contract over to YorSexual Health who offer expert and efficient service."
You said:
We should not limit LARC provision for women, but consideration should be given to how we provide this service across the city.
We did:
Working together with our Primary Care colleagues we have asked the Specialist Service at Monkgate to be the lead provider of contraception LARC, and have allocated the total budget to the specialist service.
The commissioners are committed to maintaining a contraceptive LARC service with Primary Care, to ensure that patients have a choice (where to access, who to go to for the procedure), maintain competencies in GPs and ensure service users have timely access to good quality contraceptive LARC provision.
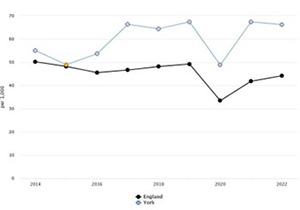
Total prescribed LARC excluding injections rate per 1000 for York
The latest data we have for total LARC prescribed (excluding injections) is from 2022 and is illustrated in this chart.
This indicates that LARC provision in York is higher than the England average, at a rate of 66.2 per 1000 women compared to 44.1 as an England average.
For Yorkshire and Humber region the rate is 52.9 per 1000 women.
A comprehensive sexual health data summary is published by UK Health Security Agency:
By working together, we are assured that GP practices and the specialist service will maintain an accessible contraceptive LARC service to the women of York. However, within the model of delivery, if there is limited provision with primary care the specialist service can pick up contraceptive LARC requests and be paid for this activity, as they cannot continue to absorb work from primary care without investment and funding.
Both commissioners and providers agree that this should be needs led and not funding led, but unfortunately sexual health budgets given to Local Authority Public Health teams direct from central government have decreased significantly over the last 11 years (since sexual health commissioning became a local authority responsibility).
Making difficult choices, including these, are the reality of those cuts to budgets. We will continue to explore every option available to increase availability of sexual health services, by looking for alternative sources of funding and new initiatives including the Women’s Health Hubs and how they can support contraceptive access to those that require it.


